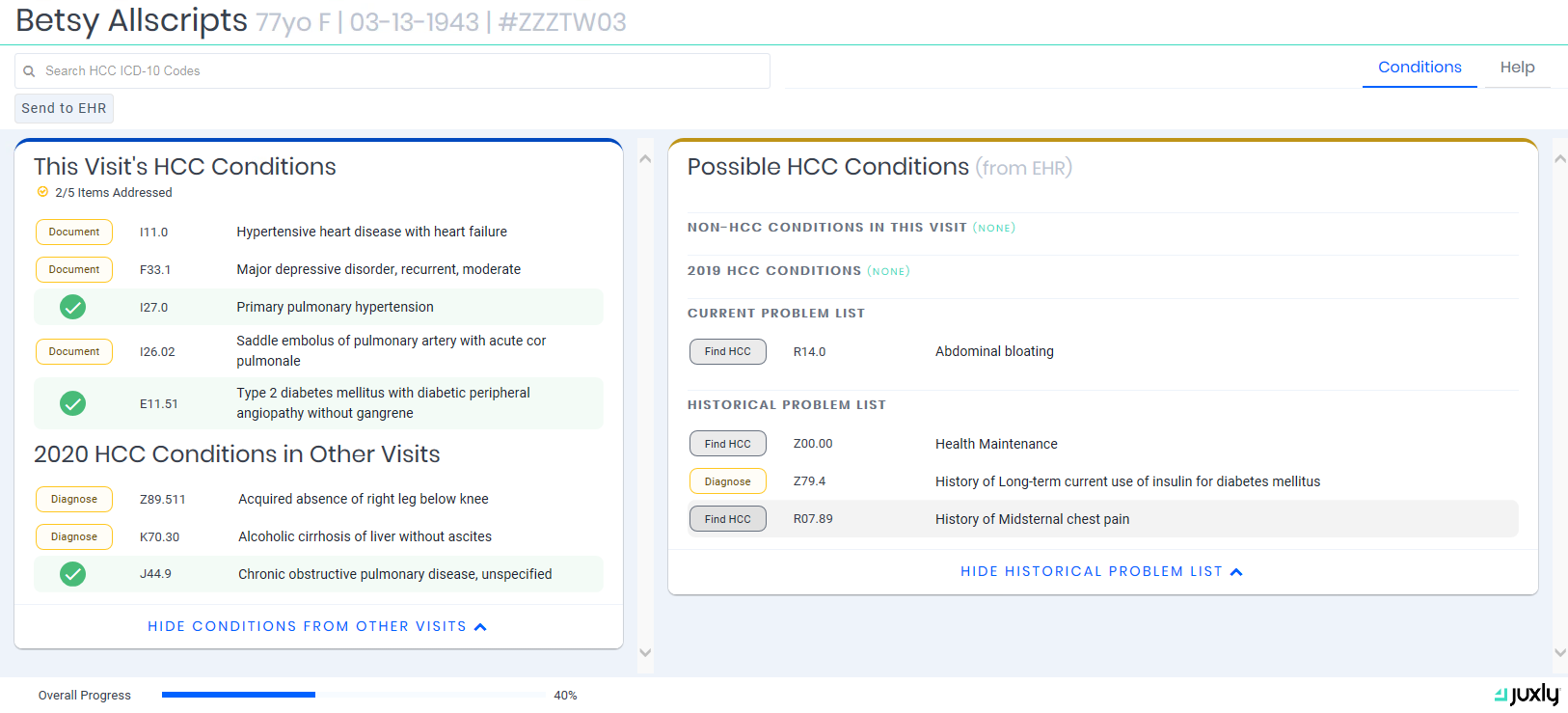
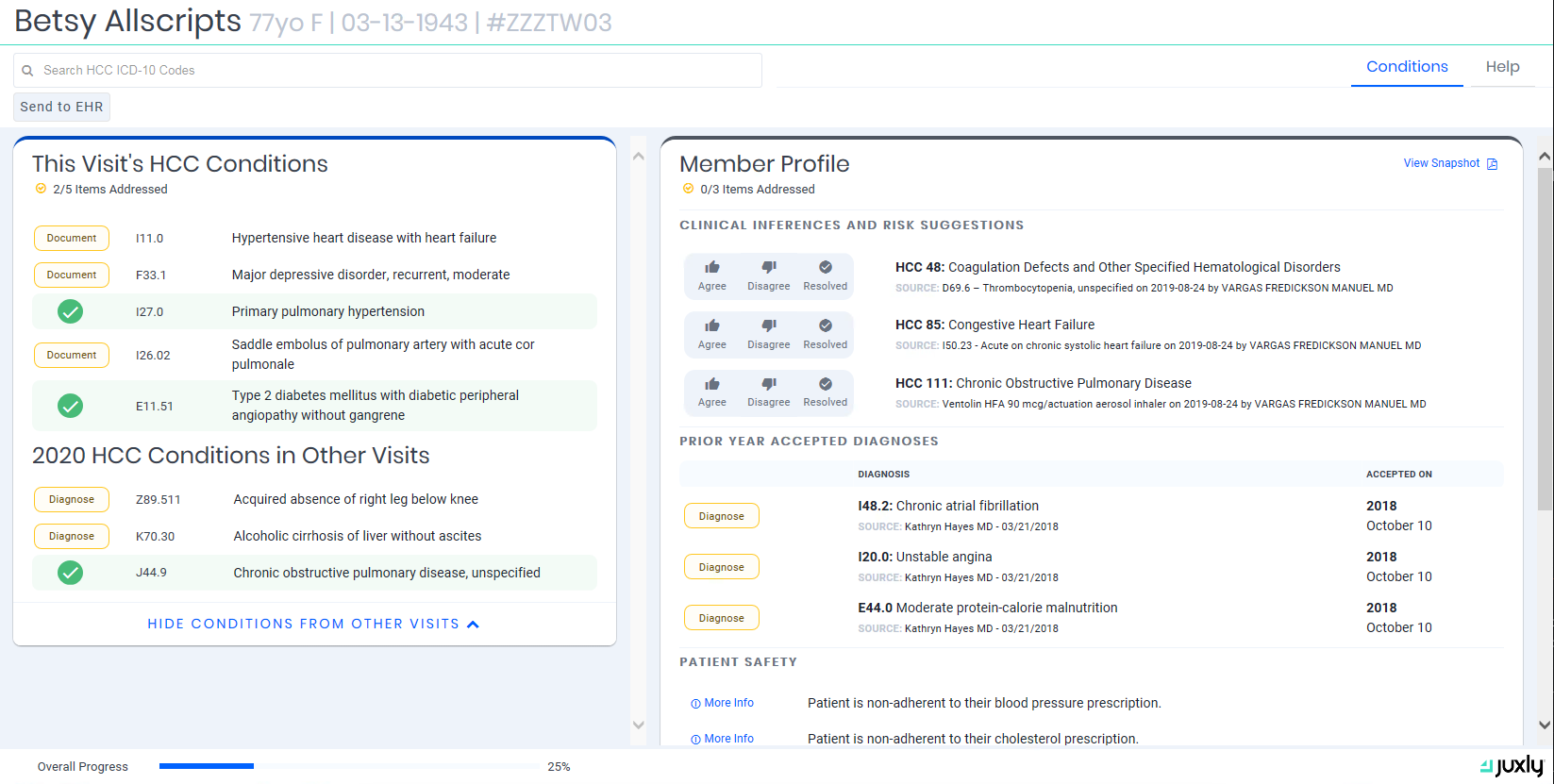
The Juxly Vault application is organized as an EHR embedded task dashboard. Worklists are generated through a combination of EHR data and work items provided by a payer.
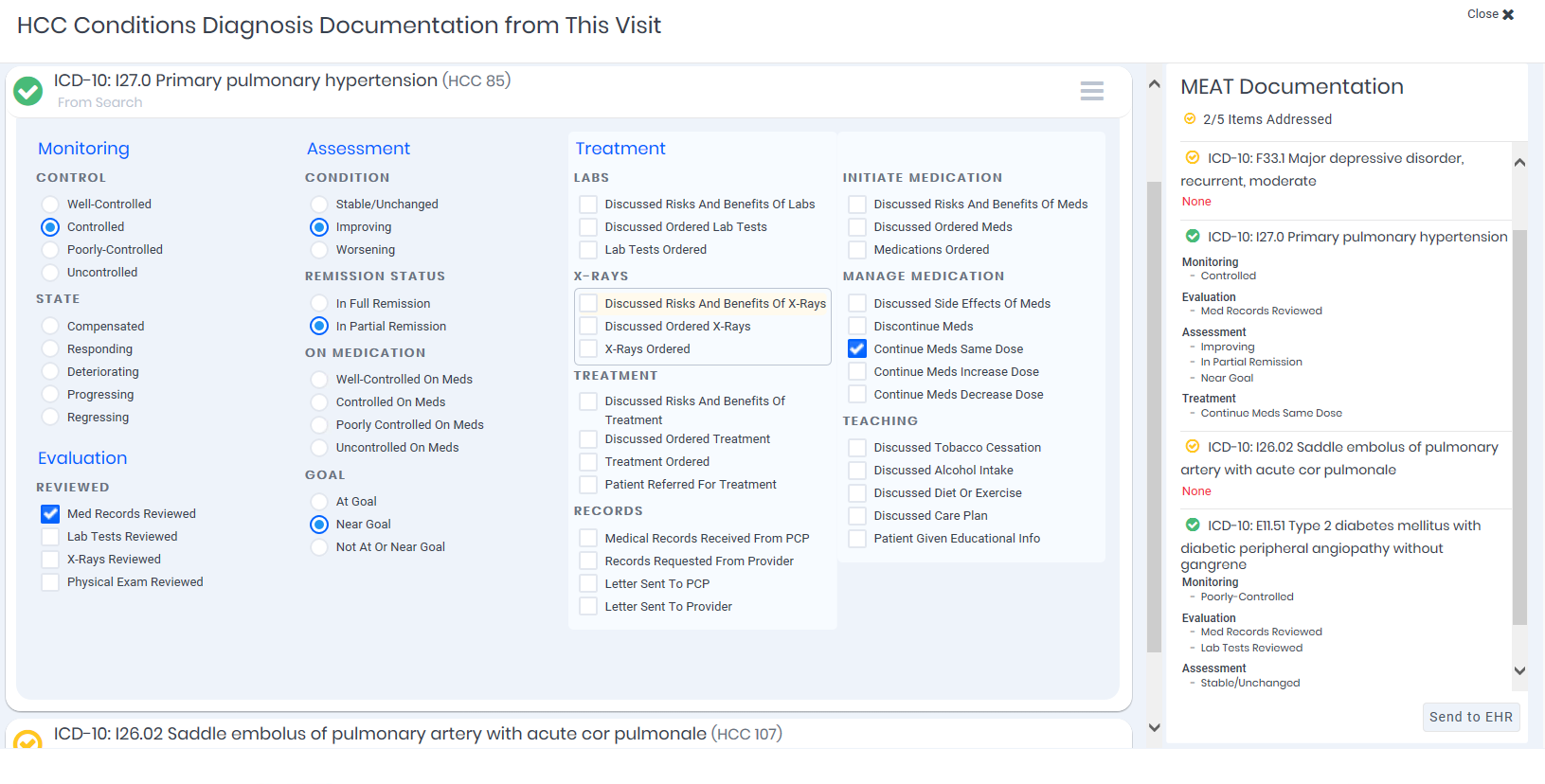
Clinical actions taken by the provider, like diagnoses or orders, are captured and stored within the host EHR, preserving the EHR as the single source of truth. Clinical information, provider actions and feedback can be sent directly to the payer in either real time or batch. Specific work lists and actions are identified during the Discovery process and implemented during the Build & Configure phase of the payer integration.
Common use cases include:
Core Platform (required)
Multi-EHR platform enabling direct engagement of providers through embedded workflows within their EHR.
Risk Suggestions
Display external risk suggestions and allow providers to diagnose and document chronic conditions at the point of care.*
Care Gaps
Display open care gaps for provider or staff review. In some EHRs, this includes reconciling an external gap list with EHR gaps and presenting a consolidated list along with the ability to initiate an order in response to a gap.*
HEDIS Discrete Data
Transparent to the user, capture current and previous year’s diagnoses, prescriptions, procedures, lab results, vital signs and immunizations for the current patient. Data is captured as discrete values and transmitted to the payer in real-time or batch format.
Care Plans
For the provider or staff to review, display the chronic conditions, care goals and actions taken by a payer coordinating the patient’s care. This can include workflow to document within the EHR that the provider has reviewed the care plan.*
Patient Care Alerts
For the provider or staff to review, display external insights into critical patient safety issues, typically related to medication adherence.*
* Includes direct feedback loop to payer on actions taken by the provider or their staff.
Additional use cases are available and supported via configuration. Custom work lists and actions can be identified during the Contracting and/or Discovery process and implemented during the Build & Configure phase of the payer integration.